What Are Migraine Triggers?
Migraines aren’t just headaches—they’re a neurological disorder with a complex mix of contributing factors. What sparks one person may barely affect another. These triggers act as the proverbial last straw, setting off chemical changes in the brain that can lead to intense pain, nausea, and sensitivity to light or sound. Nearly 16% of Americans reported having a severe headache or migraine in only three months. Environmental factors, genetics, and individual responses to daily pressures shape our risk.
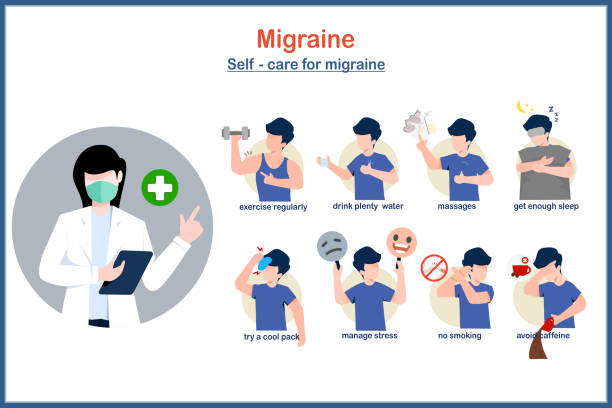
While common triggers are widely recognized, they interact uniquely with each individual. Learning to control migraines involves getting familiar with your triggers and adopting preventive strategies. Many have found that resources such as migraine treatment Jacksonville, FL, can provide actionable steps for reducing episodes and managing symptoms. These external sources deliver crucial advice and reassurance that those debilitating headaches can be significantly reduced with understanding and consistent effort. Keeping a migraine diary can be especially helpful in identifying patterns and avoiding future attacks. Stress management techniques like meditation, regular sleep, and dietary adjustments also play a vital role in prevention. Living well despite migraines is possible with the proper support and a tailored approach.
Common Triggers To Watch For
While migraines may feel unpredictable, a pattern of consistent culprits underlies most attacks. Stress, the most cited trigger, often comes from significant life changes and everyday hassles. Sleepless nights or drastic shifts in sleep routines can destabilize the brain’s ebraibrain ‘sium for pain. Food is another big piece of the puzzle, with certain ingredients like aged cheeses, chocolate, processed meats, foods containing MSG, and artificial sweeteners being notorious offenders.
- Emotional or work-related stress
- Lack of or poor quality sleep
- Certain foods (cheese, cured meats, chocolate, and foods with MSG)
- Alcohol, especially red wine and beer
- Fluctuations in hormones, particularly in women during menstrual cycles
- Bright or flashing lights, loud noises, and strong smells
- Rapid shifts in weather or barometric pressure
- Missing meals or becoming dehydrated
Research highlighted by the National Institutes of Health shows that stress isn’t a mere nuisance but can trigger migraines directly and sometimes make the brain more sensitive to other triggers. That insight suggests that management strategies can be more targeted by recognizing stress as a root problem. Being aware of these common triggers is the foundation for meaningful long-term change.
How Lifestyle Choices Make A Difference
Thoughtful lifestyle adjustments are among the most powerful levers for migraine management. Quality sleep, for example, does more than rest the body—it helps regulate the brain’s functions. Establishing a predictable bedtime and morning routine can signal to the body and mind that it’s time to wind down and recharge. Studies support that people who avoid sporadic sleep schedules have fewer and milder migraines.
Physical activity need not be intense. Even moderate exercise, such as daily walks, low-impact stretching, or gentle yoga, increases circulation and balances neurotransmitters in the brain. Small changes, like stepping outside for natural sunlight or taking short breaks to stand and stretch, can pay off in fewer and less severe attacks. Additionally, minimizing evening screen time and lowering sensory input, such as turning down bright indoor lights, may offer added defense for those whose brains are easily overstimulated.
Tracking And Identifying Your Triggers
Since no two migraine sufferers have precisely the same set of triggers, self-exploration is critical. A migraine diary is not just a log; it’s an effective way to pinpoint invisible patterns. Write down meal times, menus, hydration, weather, activity, mood, and sleep. Were you especially stressed? Did you try new foods or adjust your schedule?
Reviewing several weeks of notes often uncovers cycles or hidden culprits. For example, you might notice that migraines appear more frequently after late nights or following meals containing processed or salty foods. There are also digital solutions—many mobile apps can automate parts of tracking and even alert you to connections. Over time, the process leads to self-advocacy: you can anticipate and avoid triggers rather than constantly reacting to headaches.
Nutrition And Hydration Tips
Food and fluids can both spark and soothe a migraine. Nutrition experts urge a regular eating schedule, as skipping meals is a common trigger. Favor whole, minimally processed foods and beware of hidden nitrates, nitrites, artificial sweeteners, and foods high in sodium.
- Eat consistent meals to keep blood sugar steady.
- Limit processed foods and avoid additives such as MSG or aspartame.
- Moderate caffeine instead of quitting abruptly to avoid rebound headaches.
- Carry a water bottle. Most adults need at least eight cups of water daily, with more in hot weather or during exercise.
Proper hydration also helps flush toxins and reduces the risks of dehydration-related headaches. If you find it challenging to drink enough plain water, herbal teas, or adding fruit slices can help keep hydration interesting and compelling.
Steps To Manage Stress
Because stress is deeply intertwined with migraine frequency and severity, implementing routines that foster calm is essential. Simple techniques can help: morning and evening rituals that include five minutes of deep breathing or mindfulness, for example, can have a measurable effect. Guided relaxation tracks, progressive muscle relaxation, or gentle rhythmic movement activate the rest and digest branch of the nervous system, counteracting the overdrive caused by constant stress.
- Develop a five-minute daily meditation practice, using free online resources or apps.
- Write out your most significant worries or stressors to gain perspective and reduce mental clutter.
- Integrate stretches or mindful movement before heading to work or bed.
- Commit to small pleasures—listening to music, reading a favorite book, or connecting with a friend.
- Set realistic expectations for yourself when possible to avoid building up unnecessary pressures.
Even busy schedules can accommodate micro-breaks for relaxation. Many find that the more consistent the routine, the less likely stress snowballs into headaches. While you cannot erase all stressors, learning to manage them lessens the likelihood they’ll turn into migraines.
Getting Support And Finding Answers
Managing migraines shouldn’t feel like a solitary journey. Connecting with others—whether through migraine-specific support groups, online communities, or trusted friends and family—can offer powerful encouragement and emotional validation. Simply knowing you’re not alone in your struggle can ease the isolation that often accompanies chronic pain. These communities also serve as rich sources of practical, real-world tips you won’t typically find in medical journals—everything from go-to relaxation techniques to advice on balancing work and family during a migraine episode.
Maintaining open communication with those around you also empowers you to advocate for meaningful environmental changes, like dimming harsh office lights or taking breaks during lengthy meetings. When people understand your needs, it becomes easier to create a supportive atmosphere that prioritizes your well-being.
When To Seek Medical Guidance
If migraines escalate, change in character, or persist despite active management, seeking professional advice is essential. Medical providers can assess for underlying conditions, recommend preventive medications, and explore newer therapies—such as targeted nerve blocks or biofeedback—that may work where other avenues have failed.
When preparing for an appointment, bring your symptom diary and an honest list of what has and hasn’t worked. This information hasn’t streamlined your provider’s development of a tailored plan, often combining lifestyle interventions with medication or other therapies. Timely interventions are critical, especially for those whose attacks interfere with work, relationships, or daily functioning. Collaborative medical care offers the best hope for long-term, meaningful relief in combination with resources about migraine treatment.
Consistent, personalized strategies can help you control migraines for a long time. Stay observant, open to new ideas, and connected to community and expert resources, and you’ll be equipped to improve your daily life.